
During a checkup with her obstetrician, Marilyn Hayes tells him about overwhelming exhaustion and possible symptoms of postpartum depression, such as feeling unsafe. Hayes, a Black woman, grows increasingly frustrated as her white, male physician, Dr. Richard Flynn, dismisses her symptoms and ignores her wishes when she refuses medication. Hayes becomes visibly uncomfortable when Flynn touches her without permission and makes comments steeped in Black stereotypes, such as assuming that she’s unmarried and the baby’s father is uninvolved with her and their infant.

While Hayes and Flynn are fictional characters depicted in a virtual reality video, Hayes’ experiences are similar to those of many Black women and women of color when they interact with clinicians and their staff members, studies have found. Hayes’ checkup with Flynn is the first in a series of three virtual reality training modules being developed to heighten physicians’ awareness of implicit bias in patient care and cultural competency skills.
“Ultimately, this virtual reality training system could become a viable tool for practicing communication with diverse patients across different types of health care professions,” said Charee Thompson, a professor of communication at the University of Illinois Urbana-Champaign who studies physician-patient communication and is one of the team members developing the training series.
“There’s no reason why nurses couldn’t also use this across different health care contexts — not just for Black maternal health, but chronic pain, diabetes or some of these other health issues in which we know that there are disparities based on markers of difference such as race or class,” she said.
Thompson is the first author of a study about the project, published in Health Communication. She and her co-authors Mardia Bishop, a professor in the same department at the U. of I.; and obstetricians and gynecologists Dr. Tiffani Dillard of Carle Foundation Hospital in Urbana, Illinois; and Dr. Joseph Maurice of Creighton University School of Medicine in Omaha, Nebraska, are leading the team that is developing the modules.
The first module, which focuses on Black maternal health care, was tested in a pilot study with 30 medical students and resident physicians. Prior to and after viewing Hayes’ and Flynn’s interaction, the study participants completed a survey that taps into physicians’ beliefs about the value of eliciting patients’ opinions about the cause of their illnesses and how it affects their lives, and whether physicians can provide excellent health care without asking patients for their perspectives.
“We know that disparities in Black maternal health affect or are connected to disparities for Black infants, including preterm birth and low birth weights,” Thompson said. “And so, for me, this is one of the most urgent needs when it comes to the health of women and children.”
In Flynn’s interactions with Hayes, students saw how bias and Black stereotypes affect his communication, such as when he leaps to the conclusion that Hayes feels unsafe because her husband is violent, rather than recognizing it is a symptom of depression, Bishop said.
“The video depicts the doctor going through the entire postpartum checkup, asking questions about breastfeeding, the incision, and healing. Throughout the video, the viewer can see where the provider is behaving or communicating with implicit bias and the effect this has on the patient,” Bishop said. “Sometimes it can be difficult to recognize bias or realize that what one is saying or doing demonstrates bias. This video shows the many ways that implicit bias can enter a discussion with a patient.”
According to the post-training survey, participants’ awareness of implicit bias, their attitudes toward culturally competent communication, and their confidence in their individual communication efficacy significantly increased after the training, Thompson said.
Two open-ended questions on the survey asked participants how they would provide more empathic, individualized care for Black postpartum women. The participants responded that they were committed to building rapport with patients by prioritizing their concerns and feelings, allowing patients greater opportunities to express themselves and engaging in shared decision-making. Participants said they would listen more attentively, be more aware of their own body language, display compassion and empathy, and pay attention to patients’ verbal and nonverbal cues.
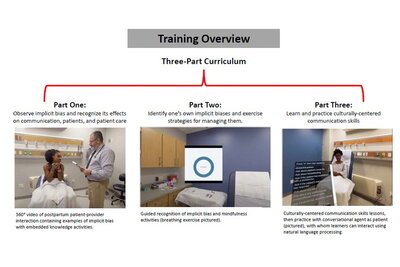
The second virtual reality training module — which is still under development, along with a third module — promotes self-reflection by helping medical students identify their own biases and learn how to mitigate them, Thompson said. In the third module, students will practice their intercultural communication skills through interactions with a virtual patient.
While the cost of the first module was $40,000, Maurice said that for universities and medical schools, virtual reality training is a cost-effective option because it eliminates the need to recruit people for role playing with medical students. “It’s a lot cheaper to produce one video and show it 100 times, as opposed to hiring 100 people to role play with the students,” he said.
Creighton University awarded Maurice a $100,000 grant to implement the training at its campus in Phoenix. The grant will expand the sample population of medical students for the research to about 300 people, he said.
The Carle Illinois College of Medicine Health Maker Lab also provided funding for the project, as did the Jump ARCHES endowment through the U. of I.’s Health Care Engineering Systems Center.
Thenkurussi Kesavadas, then-founder-director of the Health Care Engineering Systems Center at the U. of I., co-wrote the paper. He is currently the vice president for research and economic development at the State University of New York at Albany.
Other co-authors included U. of I. alumni Manuel D. Pulido, a professor of communication studies at California State University, Long Beach; Corey Zeinstra, a software engineer in immersive technologies at Boeing; and M.J. Salas, a graduate student at Rutgers University.
U. of I. graduate students Déjà D. Rollins, Emily A. Mendelson, Jia Yan, Emily R. Gerlikovski, and Sarah V. Benevento also co-wrote the study.
Editor's note: This article was originally published by the Illinois News Bureau. The paper “Healing health care disparities: Development and pilot testing of a virtual reality implicit bias training module for physicians in the context of Black maternal health” was published in Health Communication.